Very Ill
1
View details
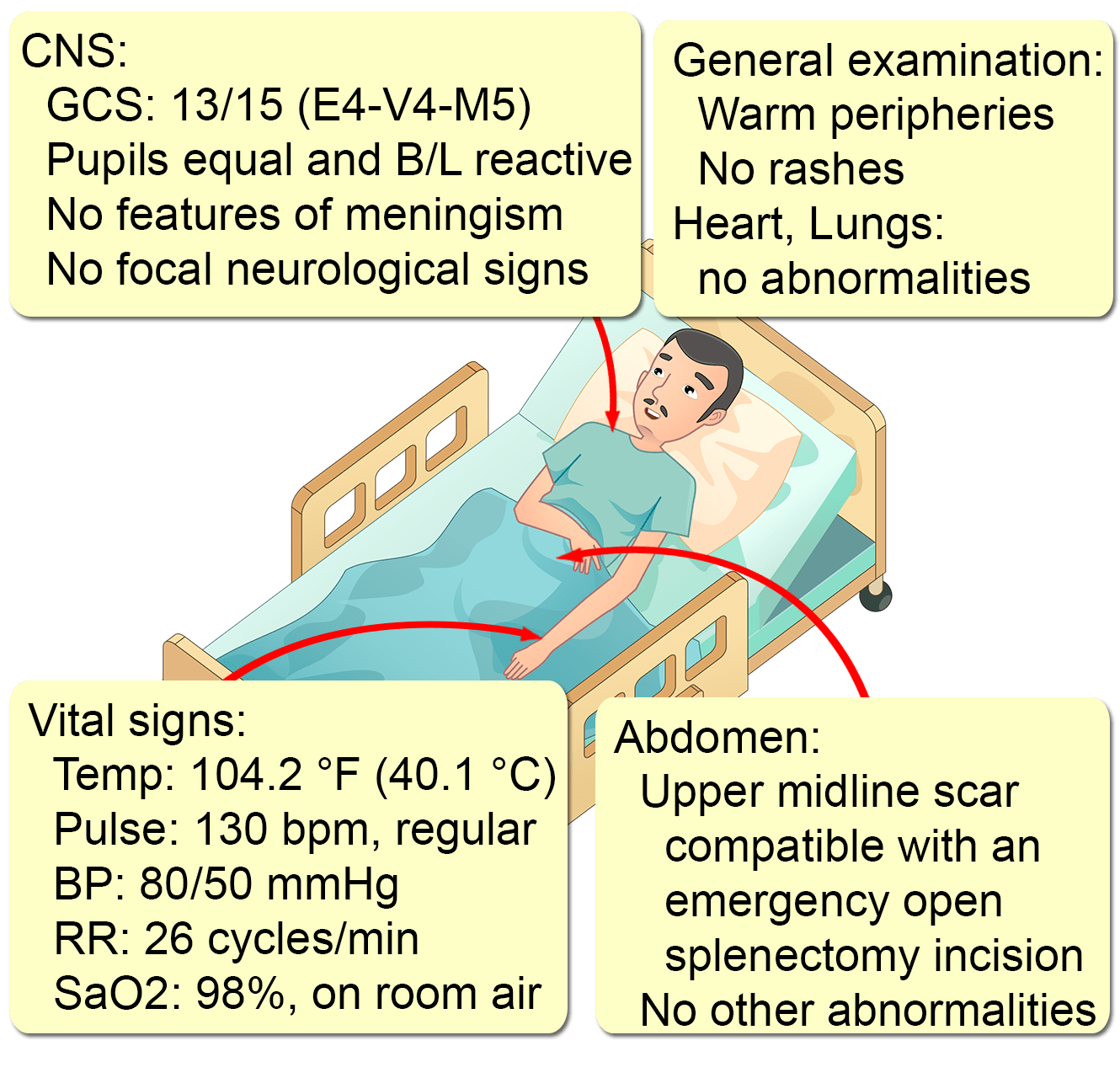
A 45-year-old man presents with altered mentation for around one hour.
He has had a fever of 104 ˚F (40 ˚C) since yesterday, in association with malaise, fatigue, and nausea. No other symptoms were present, and he did not seek medical attention, preferring to self-medicate himself with acetaminophen (paracetamol).
His medical records are unavailable, but his wife states that he had a splenectomy three years ago, following blunt abdominal trauma from a vehicular accident. She is unsure if he has received vaccination against pneumococcus, meningococcus, or H. influenzae.
He has no other comorbidities, is not on any medications, has no known allergies, does not smoke, and only drinks socially.
A complete blood count is significant for a leukocyte count of 22,000/mm3 (normal: 4,000-11,000), with 85% neutrophils. His capillary blood glucose, serum electrolytes, chest x-rays, and urinalysis are all normal.